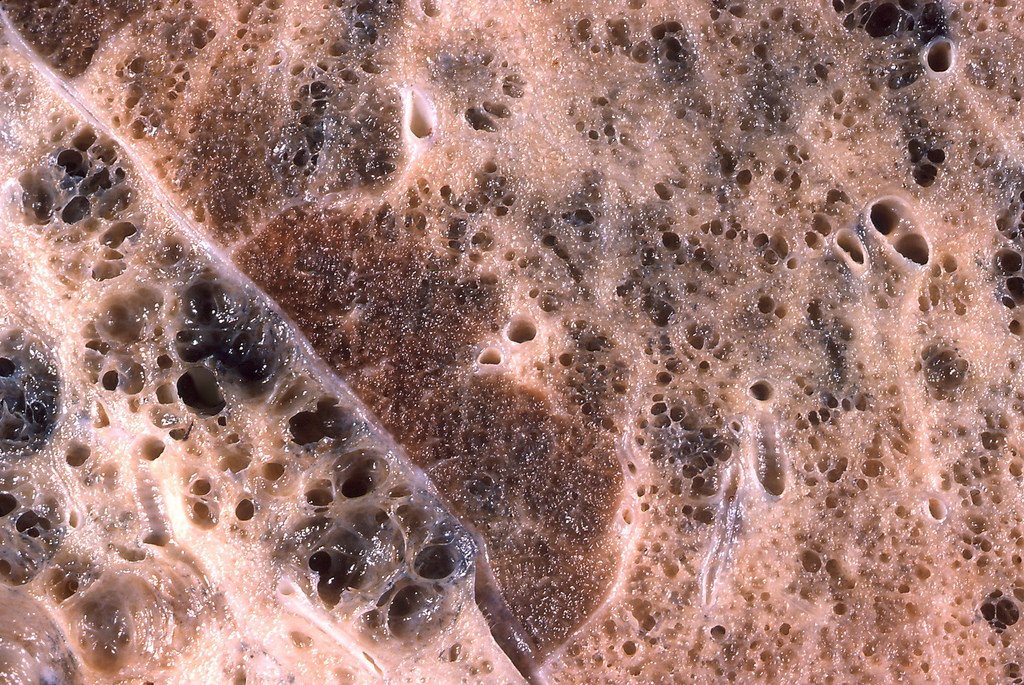

A brand new article in Sciencemag.org presents a study demonstrating how pathological fibrosis increases with age, but how NRF2 activation in mice was able to reverse the damage and repair lung capacity and fibrosis (scar tissue) resolution.
This is a promising study because the current treatments of pathological and cystic fibrosis are costly and very time consuming. Persistent fibrosis in lungs of aged mice was caused by the loss of cellular redox balance. The mice in the study with low NRF2 expression had a higher incidence of progressive lung disease. Tissues from human lung samples demonstrated this same Nox4-Nrf2 imbalance.
The abstract concludes with the following promising statement. "The studies suggest that restoration of Nox4-Nrf2 redox balance in myofibroblasts may be a therapeutic strategy in age-associated fibrotic disorders, potentially able to resolve persistent fibrosis or even reverse its progression."
Please validate any information here with a healthcare professional. The content is provided for education purposes, This content has not been evaluated by the Food and Drug Administration. Any advice or products mentioned is/are not intended to diagnose, treat, cure, or prevent any disease,










